When do I need to submit my FSA claims?
FSA Claims need to be submitted by the date and cut-offs outlined in your plan documents. Benefit Resource provides this information in the Plan Highlights, which can be found in the Documents section of the BRiWeb Participant login. You may also contact your employer benefits administrator.
How does reimbursement for orthodontia expenses work?
For a plan that allows reimbursement of orthodontia (e.g. Medical FSA), IRS regulations allow reimbursement based on date of payment, date of service or the payment due date on statements/coupons. IRS regulations allow a Medical Flexible Spending Account (FSA) participant to be reimbursed for pre-paid orthodontia services, up to a participant’s annual election amount, before […]
Can I submit a claim for a medical service before the service is provided if I have already paid for it?
No, you need to wait until after a medical service has been provided before submitting your claim. (Note the IRS exception on “How does reimbursement for orthodontia expenses work?”)
Can I submit a claim for a medical service prior to paying for it?
As long as the service was provided, a claim can be submitted for reimbursement whether or not payment has been made.
Must all my claims be submitted before the plan year ends?
No. Claims for eligible services must be received by Benefit Resource within the time frame indicated in your Plan Highlights.
How do I submit an expense for reimbursement?
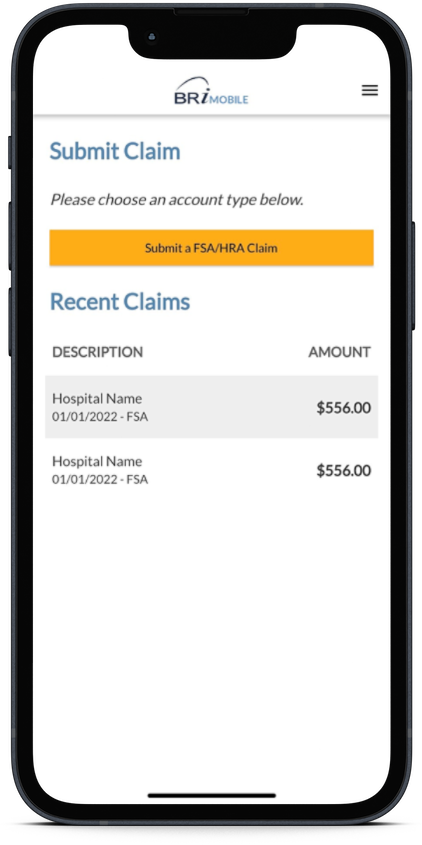
After a service is provided, you will need to submit a completed claim with supporting documentation to Benefit Resource. You can do this in one of the following ways: The BRIMOBILE app allows mobile device users to submit claims on-the-go. Log into the participant website, under the FSA/HRA Plans tab, select Submit an Online Claim. Complete […]
Is there a minimum claim submission amount?
There is no minimum claim amount, but your Plan may have a minimum reimbursement amount (usually $15). If your eligible claim amount is less than the minimum, it will be held until additional claims are submitted. (During the run-out period after the end of each plan year, reimbursements will be issued even if they are […]
If I pay my daycare center the same amount every single week, can I automatically receive reimbursement from my Dependent Care Account without submitting a claim every week?
Since eligible Dependent Care services cannot be claimed until after the service has been provided, reimbursements cannot be automatically generated to you. You can submit claims weekly or accumulate claims and submit several weeks at a time (as long as the services have already been provided).
What happens if the cash balance in my Dependent Care FSA is less than the amount of an eligible claim that I submit?
Your claim will be reimbursed up to the cash balance available in your Dependent Care FSA. You will be reimbursed for the remaining amount once additional funds are deposited into your Dependent Care FSA.
What supporting documentation do I need to submit with my completed claim for reimbursement from my Dependent Care FSA?
Acceptable supporting documentation for a Dependent Care FSA claim must include the following information: Type of service provided Date(s) the service was provided (e.g. 2/2/2012 – 2/6/2012) Name of dependent for whom service was provided Provider of the service Your out-of-pocket expense for the service.
Can I submit a Dependent Care claim before a service is provided if I have already paid for it?
No, you need to wait until after a Dependent Care service has been provided before submitting your claim. For example, if you pay a summer day camp registration in March but the day camp will be held in July, the claim for reimbursement of the March registration fee cannot be submitted until the end of […]
What supporting documentation do I need to submit with my completed claim when requesting reimbursement from my Medical FSA?
Acceptable supporting documentation for medical claims must include the following information: Name of provider of the service/product Date of service/date product was purchased Type of service/product (drug name required for prescription claims) Your out-of-pocket expense for the service/product (amount not covered or reimbursed elsewhere) Name of employee or dependent for whom the service/product was provided.
Where should I submit my claim first for medical expenses: to my insurance or my Medical FSA?
Your claim must always be submitted to your insurance carrier first. The remaining eligible expenses that you pay out-of-pocket can then be submitted for reimbursement from your Medical FSA.
Will my FSA claims be paid directly to the provider?
No, payment will be made to you. You are still responsible for paying the provider.
How long will it take to receive reimbursement for my claim?
Claim reimbursements are processed every day. Please allow 5-7 business days to receive your reimbursement. To receive your funds faster, sign-up for direct deposit through briweb.com


